My life is turned upside down: insomnia, depression, anxiety and hot flushes during perimenopause (Part 1)
You are a mid-age lady, approaching 50 years old. Life is suddenly turned upside down. You were energetic, had great memory and was switch on, then one day you suddenly find yourself being tired a lot, having poor memory, feeling not motivated or feeling anxious for no reason. The worst of it all is not able to fall asleep easily, wake up frequently throughout the night or wake up at 2 am or 3 am, then taking a long time to get back to sleep. You lie in the darkness, all thoughts trivial, unhappy, irrelevant or obsession run through your mind, keeping you awake.
If this describes you, then you are entering into menopause, and you are not alone. As mentioned in our previous blog, one in two perimenopause women experiences some forms of sleep disturbance, and one in three experiences depression or anxiety. The sleep problem gets worse after menopause (Baker et al 2018). Those who have surgical menopause due to removal of ovaries on both sides experience far worse sleep problems, reflecting the importance of a sudden change in female hormones on sleep quality. Linking to the changes in female reproductive hormone is hot flushes. Frequent hot flushes at night is closely related to perimenopausal insomnia.
Not all perimenopausal insomnia is, however, associated with hot flushes. Some insomnia is related to mood changes, such as depression or anxiety. The complex relationship among hot flushes, insomnia, and depression makes the treatment charllenging. For instance, anti-depressants used to treat depression can impact on sleep quality.
When considering peri-menopausal insomnia, one needs to consider the multiple factors, beyond those relate to hormonal changes. The diagram here describes an interdependent and interactional relationship among insomnia, hot flushes, and depression, and the many factors contributing to insomnia during perimenopause. Some factors (in blue) are related to menopause, whereas many are about women’s physical and mental health prior to menopause, lifestyles, and coping strategies. It is also important to note the significant impact from social factors during this midlife stage.
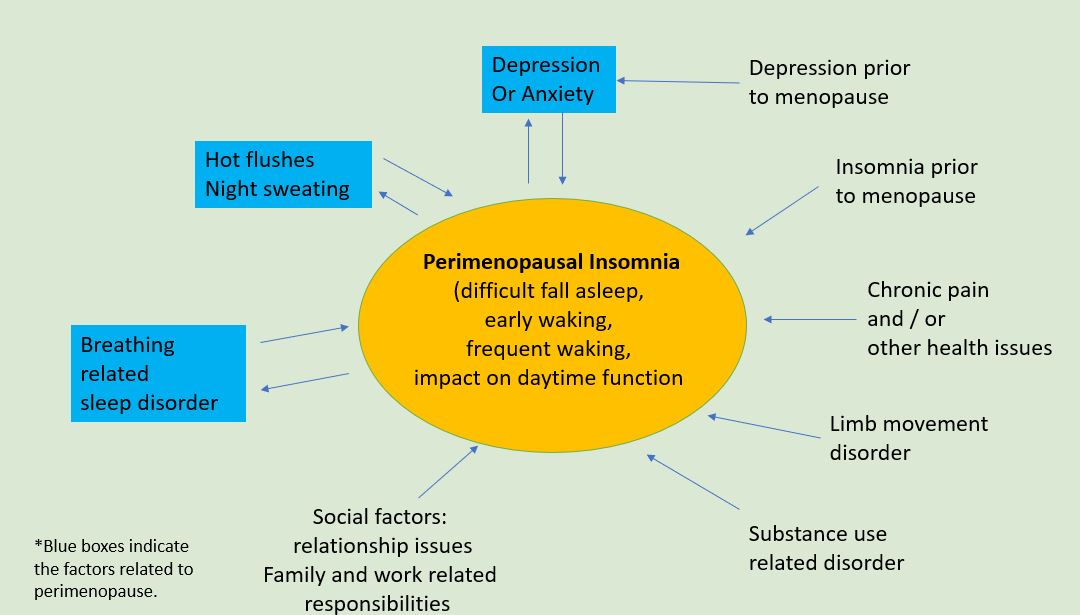
This diagram might also help you assess the specific factors related to your insomnia and how to address those non-menopausal factors. Perimenopause is the time for women to transit not only physically, but also mentally and socially. At Geelong Chinese Medicine Clinic, we encourage women to shift the transit to transform, and to not only turn the upside-down life back, but also to elevate the life to another level.
In part 2, we will talk about how Chinese medicine understands the complex interaction among hot flushes, insomnia and mood changes, and how acupuncture might provide a promising approach to comorbid depression and insomnia in perimenopause.